'It was bad.' Three hours on the Covid ICU in Seattle

KUOW's Isolde Raftery spent an afternoon on the Covid ICU at University of Washington Medical Center in Seattle.
Using her tape, reporter Joshua McNichols produced a piece to walk us through the unit, using Raftery as his guide.
Listen by clicking on the audio. Below is the story Raftery wrote earlier for KUOW.
The air turns over every 20 to 25 minutes on the Covid ICU at the University of Washington Medical Center, but no one breathes easy.
The wing is shaped like a rectangle. In the far left corner, nurses Leah Silver and Ashlee Davis tend to a man dying of coronavirus.
Silver is 25, her dark hair shaved on one side, and Davis is 32, with strawberry-blonde hair pulled into a low bun, and a tattoo of evergreen trees on her forearm. They are ECMO nurses, which means they manage a pump that functions as the patient’s heart and lungs. The machine, roughly the size of a milk crate, adds oxygen to the patient’s blood.
Silver and Davis chat in an empty patient room. Next door is their patient. The rooms are separated by windows, and they can see through to the man, whose room is white and beige and an organized mess of tubes and cords. Family photos line the windows, including one of the man, who is handsome and has his arm around a beaming woman. The poster on his door says that he is gregarious, loves to garden and be with his family.
His body is bloated now, his stomach tinged with gray, and the cotton around his mouth is blotted with blood. They do not know why his mouth is bleeding.
Few see what these nurses see: That this disease is unpredictable, and will ravage a middle-aged man’s body. This man, in his 50s, had been healthy. He thought he had a cold and then went to a regional hospital where he tested positive for coronavirus.
We do not see what they see because we are sheltered, by necessity, from the dark side of the pandemic.
We hear the sirens, and read about the parking-lot tests sites, and share in the frustration of being shut in while the flowers bloom outside, fragrant, reminding us that time marches on, and that summer approaches, and that we are missing out. We wear masks, or we don’t, because they make our glasses fog and faces feel hot. The virus is a theoretical exercise for most of us, because unless you’ve had it, or have lived with someone suffering through it, the virus is invisible.
And so we do not see what these nurses see, the horrors of the pandemic: The bodies unconscious, mostly naked, covered by towels, ventilators taped tight over faces.
We do not see the deaths by Zoom, or the nurses who must surveil their patients by baby monitor, because it is too dangerous to duck into rooms more than a few times a day.
We do not watch the agonizing FaceTime conversations that relatives endure, because they are not allowed onto the floor, and there is no other way to show their love.
We do not hear the mothers cry when they learn their adult children have died, and that they have died alone, because it would have been too dangerous for them to be there, holding their child’s hand in those final moments.
We do not see the nurses outside their patients’ rooms, after the machines have been turned off, because protocol demands that they wait one hour after death to enter, lest the virus linger and infect them and anyone standing in the hallway.
The nurses say they feel secure here on the Covid ICU, that it is the safest place on earth right now because of the air filtration, and because they know who has the disease. Unlike the grocery store, they say, where anyone could be sick, and all they have for protection is a mask.
“It’s probably the freshest air you can get anywhere,” Silver says, and Davis nods. It is a mantra on this unit, an unexpected logic: Here, where people are dying of coronavirus, it is safe; outside, where the virus is invisible, it is unsafe.
It sounds like denial until the nurses discuss the seriousness of the virus.
“I don’t think the media is portraying it as seriously as it is,” Silver says. “At least, when I hear my friends, or people not in health care, talk about it, their reaction is, ‘Oh, I’m in my 20s, I’m in my 30s, I run every day.’ Well, this disease doesn’t care.”

The nurses speak of the joys, too. Breaks in the sun, and returning with treats for coworkers, like small bags of Cheez-Its and crunchy Chips Ahoy.
And the biggest joy: Patients who recover and are wheeled out to “Girls Just Wanna Have Fun” jamming from a speaker, and a community that has rallied around them with 8 p.m. cheering, sidewalk chalk messages of support, amateur parades, and boxes of restaurant food.
They feel held up by the community, and by each other, but this virus has chewed on their nerves and taken away their patients.
“It does affect us, with Covid,” Silver says. “In some ways, the deaths have been more frequent that they would be normally.” It doesn’t get easier the more people who die, she says. It gets harder.
She mentions a study she read: Of 1,257 nurses in Wuhan, China, where the pandemic started, 50 percent wound up with depression or anxiety after working on the frontlines, many of them caring for Covid patients
“It’s a whole different kind of nursing,” Silver says.
The nurses plan their 12-hour shift to limit how often they go into a patient’s room.
On this day, Silver dons a gown and helmet-like hood as Davis watches. She straps on an air purifying device. Davis checks its battery and the air flow, and touches the hose that sticks out the back of Silver’s hood.
“Let me see your face,” Davis says, intensely focused on her colleague. And then she is satisfied, and greenlights Silver to enter their patient’s room.
Upon entering, Silver first looks at her patient. “You don’t know what he’s going to look like,” she says. “We’ve been using Zoom and baby monitors to monitor what the patient is looking like, to keep it safe for us.”
Silver tells him that he is safe, where is he, and who she is.
“I know that if I was in that bed, terrified and in restraints, alone, I’d want to know where I am, who’s talking to me, and trying to manage my pain,” she says. “I try to speak to them if they were me.”
The man has had setbacks, and his lungs have become inflamed. He has been paralyzed with medicine to help his body do less work.
When Silver cleans his mouth, he blinks, as though surprised.
“Be strong,” she tells him. It’s his personal motto, one his family have asked the nurses to say to him. And then Silver leaves. She is sweaty from the stress.
Davis waits for her outside, herself in full protective gear. She helps Silver take off the hood, and as she lifts it off, Silver exhales audibly with relief.

“Have you seen Chernobyl on HBO?” Silver asks. “That part, ‘These are the most important 90 seconds of your life?’ That’s what this feels like.”
She is referring to the young Soviet men who cleared debris from a rooftop after the Chernobyl disaster in 1986. They each had 90 seconds on the roof.
In this case, the tension is around the chance that the circuit could break, causing the virus to aerosolize in the room.
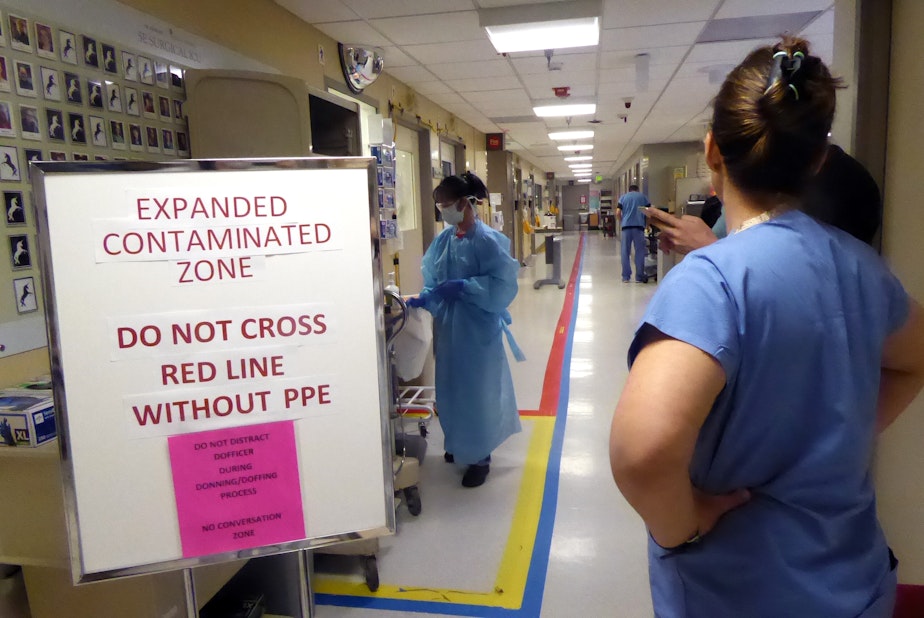
Down the hall, Amy Haverland, the nurse manager on the Covid ICU, watches another nurse pull on protective gear. They’ve been lucky here on the Covid ICU and have the protection they need.
This physical unit is Haverland’s home base, but the team is different.
“February 29, I was at a birthday party, and I got a call from my director to say they had found the Covid patients in Kirkland, so things were about to start changing,” she says, standing in the hallway.
There are 14 rooms in the Covid ICU, an older unit at UW Medicine. At the beginning, four rooms had negative air pressure. A crew converted the other 10 in a day or two.
“And then patients started coming in,” Haverland says.
In the room behind her, a woman from eastern Washington regales nurses with her story of getting the painful Covid nasal swab. The woman, whose name is Theresa, is chatty and funny. She is not sick enough for the Covid ICU, so they send her to an acute care ward.
“It’s so bizarre,” Haverland says, “because people are doing fine, doing fine, doing fine and then all of a sudden” – she snaps her fingers – “they’re not. You try to make assignments and figure out where to put people, but you have no idea which day someone is going to start getting better, or that’s the day they get significantly worse.
“That’s the part that shakes you up about this virus,” Haverland says.
A week or so later, Public Health Seattle & King County releases the names of people who have died in the previous few days – everyone, not just those who had coronavirus.
A single line from the last week of April is for the family man who loved to garden, Silver and Davis’s patient, whose motto was “Be strong.”
The audio version of this story includes music by the band Gentlemen Writers.





